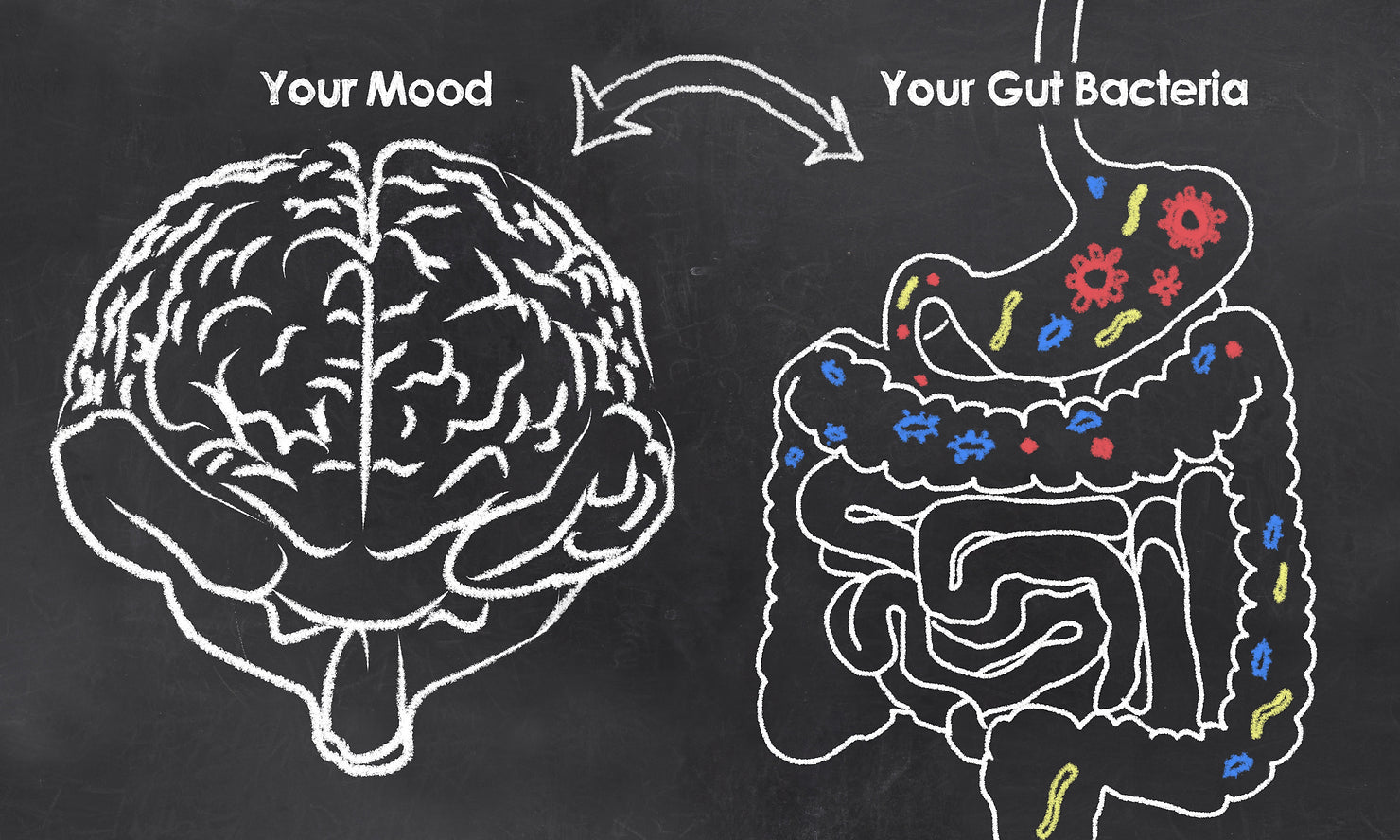
It is becoming increasingly apparent that the health of our gut and the health of our brain are intimately linked. Depression, anxiety, and panic disorders are on the rise, and we are also seeing a similar increase in intestinal disorders, autoimmune diseases, and metabolic imbalances. Recent research has shown that there is a connection between what we eat and the health of our brain and gut.
The gut is often referred to as the "second brain" due to the presence of thousands of nerves that are connected to the central brain via the vagus nerve. This nerve is the longest nerve in the body and plays a crucial role in the communication between the brain and the gut. Messages from the brain travel down the vagus nerve to the gut, signaling a sense of calm or distress, while messages from the gut travel up the nerve to the brain, indicating its well-being or state of distress.
This communication requires molecular messengers known as neurotransmitters, which play a crucial role in our memory, feelings, and most bodily functions. Imbalances in neurotransmitters have been linked to depression, anxiety, and other mood disorders. Our diet, environment, and moods can impact the type of neurotransmitters we produce.
Recent research has highlighted the role of intestinal bacteria in influencing anxiety and depression. These tiny organisms reside in our gut and have a significant impact on brain development, cognitive formation, immunity, and many organic pathways. When our intestinal flora is balanced, it can lead to balanced emotions and thoughts. Dysbiosis, or imbalance, can lead to emotional imbalance and mood disorders. Various factors, such as genetics, lifestyle, birth, and medications, can affect the quality of our gut-ecosystem.
Dietary factors play a crucial role in maintaining a healthy gut-ecosystem. Plant-based fiber derived from fresh fruits, vegetables, legumes, and whole grains produce short-chain fatty acids (SCFA), which fuel bacteria. SCFA then activate the production of serotonin in the gut, which travels up the vagus nerve and stimulates a sense of peace and contentment. Studies have shown that those with high SCFA have less circulating cortisol (a stress hormone) and are less prone to anxious and depressive thoughts and actions.
On the other hand, some popular foods lead to imbalanced mood and poor memory. High sugar consumption has been linked to impaired memory and diminished cognitive processing. Caffeine stimulates a stress response, which can diminish blood flow to the brain. Trans-fats found in processed pastries, fried and junk foods, result in chronic inflammation leading to oxidative stress in the brain.
The balance between our brain and gut health is dependent on our diet, lifestyle, and intestinal microflora. It is essential to detoxify our brain of negative thoughts and critical attitudes while cleaning our intestinal tract of toxic influences. A healthy gut leads to a healthy brain, and the two are intimately linked. By choosing a diet rich in whole, plant-based foods, we can help support the health of both our gut and our brain.
---
Ready to heal your gut? Try Aurum Alive today!
---
Remember to consult with your healthcare provider before making any changes to your diet or lifestyle.
---
REFERENCES: 1. Carabotti M, Scirocco A, Maselli MA, Severi C. The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann. Gastroenterol. 2015;28:203–209. 2.Javier A. Bravo, et al. Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. PNAS 2011 : 1102999108v1-201102999. 2. Lyte, M. Probiotics function mechanistically as delivery vehicles for neuroactive compounds: Microbial endocrinology in the design and use of probiotics. Bioessays. doi: 10.1002/bies.201100024. 4. Hurley, Dan. Your Backup Brain. Psychology Today. Dec 2011. 80 - 86 5. Am J Physiol Gastrointest Liver Physiol. 2013 Jan 15;304(2): G211-20. doi: 10.1152/ajpgi.00128.2012. Epub 2012 Nov 8. 6. Lakhan, Shaheen, Kirchgessner A. Gut inflammation in chronic fatigue syndrome Nutrition & Metabolism, Oct 12, 2010. DOI: 10.1186/1743-7075-7-79 7. Diaz Heijtz R, Wang S, Anuar F, Qian Y, Björkholm B, Samuelsson A, Hibberd ML, Forssberg H, Pettersson S. Normal gut microbiota modulates brain development and behavior. Proc Natl Acad Sci U S A. 2011 Feb 15;108(7):3047-52. Epub 2011 Jan 31. 8. Clarke G, Grenham S, Scully P, Fitzgerald P, Moloney RD, Shanahan F, Dinan TG, Cryan JF. The microbiome-gut-brain axis during early life regulates the hippocampal serotonergic system in a sex-dependent manner. Mol Psychiatry. 2012 Jun 12. doi: 10.1038/mp.2012.77. [Epub ahead of print] 9. Longhi R, Almeida RF, Machado L, Duarte MM, Souza DG, Machado P, de Assis AM, Quincozes-Santos A, Souza DO. Eur J Nutr. 2017 Apr; 56(3):1003-1016. Epub 2016 Jan 11